A groundbreaking study suggests that liquid biopsies, a non-invasive blood tests may significantly enhance the care of people with metastatic breast cancer, especially those whose tumors are driven by estrogen. The findings indicate that liquid biopsies can detect changes in cancer cells months earlier than traditional imaging methods, allowing for timely treatment adjustments and potentially prolonged disease control.
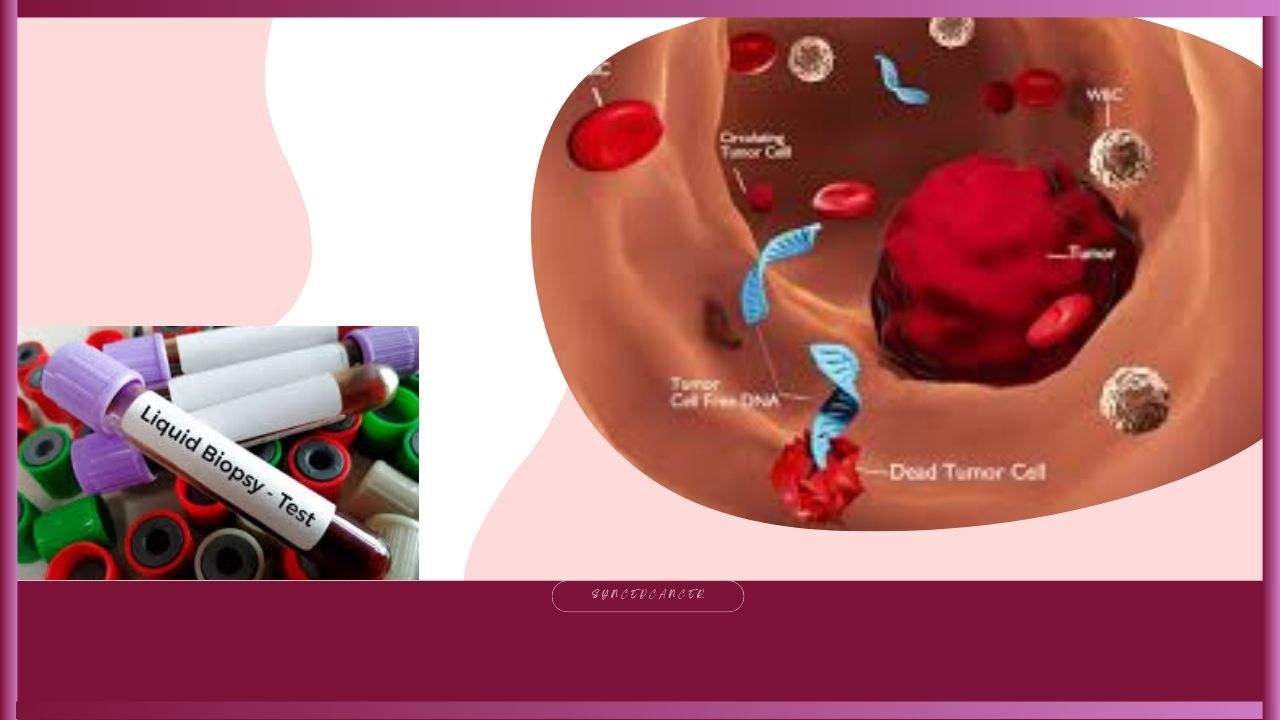
Liquid biopsies are highly sensitive blood tests that detect small fragments of tumor DNA or circulating cancer cells in the bloodstream. Unlike conventional imaging or tissue biopsies, these tests are non-invasive and can reveal genetic mutations in cancer cells even before symptoms appear or tumors enlarge. While Liquid biopsies have not yet replaced standard screening methods like mammograms or colonoscopies, their role in advanced cancer management is growing.
The new research, published in The New England Journal of Medicine and presented at the American Society of Clinical Oncology (ASCO) annual meeting in Chicago, focused on people with metastatic breast cancer fueled by estrogen. This form of cancer is typically treated with drugs that target specific estrogen-related proteins. However, when these proteins mutate, current treatments may stop working, causing the cancer to progress.
Dr. Nicholas Turner, co-author of the study and a professor of molecular oncology at the Institute of Cancer Research and The Royal Marsden Hospital in the UK, emphasized the significance of early detection through liquid biopsies. “By identifying mutations early, we can switch patients to a more effective treatment before their cancer worsens,” he said.
Oncologists monitor treatment effectiveness through imaging scans like CT or PET every three months. These scans help determine whether tumours are shrinking or growing. However, Turner’s team found that liquid biopsies could detect key mutations up to nine months before they would be visible on scans. This offers a critical opportunity to replace ineffective treatments sooner.
In the study, 315 patients with estrogen-driven metastatic breast cancer were enrolled. All had developed mutations that could compromise their current therapies. Researchers randomly assigned half to immediately switch treatments based on liquid biopsies results while the other half continued their usual regimen.
Among those who changed therapy early, their hormonal medication was replaced with camizestrant, an experimental drug not yet approved by the FDA—camizestrant works by blocking estrogen’s ability to fuel cancer growth. The trial was funded by AstraZeneca and supported by early research from the U.S. National Institutes of Health, according to co-author Dr. Massimo Cristofanilli, director of breast medical oncology at Weill Cornell Medicine and NewYork-Presbyterian Hospital.
Results showed that participants who switched to camizestrant had a median progression-free survival of 16 months, compared to 9 months in those who stayed on their previous medication. After one year, 61% of early-switch patients still had stable disease, versus only 33% of those who didn’t change therapy. At the two-year mark, 30% of early-switch participants remained stable, compared to just 5% in the delayed group.
Beyond controlling tumor growth, those who changed therapies earlier also reported better overall health and quality of life for up to 23 months. In contrast, participants who remained on their initial medications reported declines in health and well-being after just 6.4 months.
Dr. Turner noted, “If we switch treatment at just the right time, we can keep the cancer asleep and the person well. Many of my patients can continue working and enjoy life with their families.”
While camizestrant was associated with more side effects than standard hormonal therapy, it was generally well tolerated. Only 1.3% of patients discontinued camizestrant due to adverse effects, compared to 1.9% in the standard drug group.
Side effects included reduced white blood cell counts, a slower heart rate, and visual disturbances like flashes or floaters. Despite this, the majority of participants continued using the drug.
Although camizestrant is still under investigation, the FDA has already approved a similar drug called Faslodex, offering another option for patients needing a change in treatment.
Expert Opinions and Remaining Questions
Dr. Heather Parsons, a medical oncologist at Dana-Farber Cancer Institute and assistant professor at Harvard Medical School, praised the study but urged caution. “This is an important study, but the results are still early. We need to determine whether switching therapies early helps patients live longer or exposes them to stronger drugs sooner,” she said.
Indeed, a central unanswered question is whether early intervention improves long-term survival. Dr. Turner will continue monitoring the study participants to answer this critical question.
Currently, patients with metastatic breast cancer typically live an average of five years after their cancer spreads. Demonstrating an actual survival benefit may take several more years of follow-up. Additionally, the study’s participants were primarily white, raising questions about how well the findings apply to other racial and ethnic groups.
Dr. Kelly Shanahan, a physician living with metastatic breast cancer since 2013 and president of METAvivor, an advocacy group, called the findings “exciting and compelling.” She added, “If I were in this situation, I would want to discuss early switching with my oncologist—especially if the side effects were manageable.”
Broader Potential: Liquid Biopsies Beyond Breast Cancer
The promise of liquid biopsies isn’t limited to breast cancer. A 2022 study in The New England Journal of Medicine led by Dr. Jeanne Tie in Australia used similar blood tests to identify which early-stage colon cancer patients needed chemotherapy after surgery and who could safely skip it. Although availability varies by region, these tests are used in some clinical settings.
Liquid biopsies are also being explored for early cancer screening. The FDA recently approved a blood-based colorectal cancer screening test called Shield. While not a replacement for colonoscopy, Shield identified 83% of colon cancers in trials. However, the test has not yet been shown to save lives, and major health organizations have yet to endorse it.
Dr. Cristofanilli expressed hope that liquid biopsies might also complement mammograms, especially for women with dense breast tissue where tumors may be harder to detect. “This technology could eventually reduce the need for painful needle biopsies and provide more accurate diagnostics,” he said.
References
NBC News – ‘Liquid biopsies’ alert advanced breast cancer patients when new drugs are needed
Accessed 22nd June,2025










What do you think?
It is nice to know your opinion. Leave a comment.